Abstract
IntroductionBCR::ABL1-like acute lymphoblastic leukemia (Ph-like ALL) accounts for approximately 25-30% of B-ALL and belongs to the high-risk group. In most literature, patients with Ph-like ALL are resistant to chemotherapy. Most Ph-like ALL with ABL class rearrangements have been reported to be sensitive to tyrosine kinase inhibitors. The optimal treatment of patients with other types of Ph-like ALL remains unknown. Anti-CD19 CART therapy has been reported to overcome high-risk cytogenetics in B-ALL. Currently, there are few data on anti-CD19 CART in patients with Ph-like ALL. Here, we present the clinical features of Ph-like B-ALL patients who underwent CART cell therapy and allogeneic hematopoietic stem cell transplantation (allo-HSCT) in a single center in China .
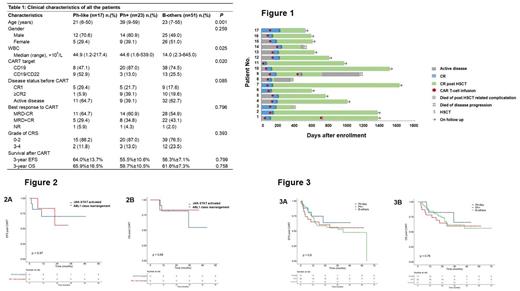
MethodsThis study included17 patients diagnosed with Ph-like B-ALL, 23 patients with Ph-positive ALL and 51 patients with other B-ALL patients were included from Jan, 2018 to Nov, 2020 at the First Affiliated Hospital of Soochow University. All patients accepted autologous anti-CD19 CAR T-cell therapy and subsequently allogenic stem cell transplantation. Kaplan-Meier method was applied to estimate patients’ survival. Event-free survival (EFS) was defined since the date of enrollment to the date of evidence of no response, relapse or death due to any causes. Overall survival (OS) was defined since the date of enrollment to the date of death due to any causes. The patients in this study were from clinical trials NCT03275493 and NCT03614858. This study was approved by the institutional ethical board and was performed with written informed consent were taken by the patients or their parents.
ResultsEleven patients harbored ABL1 class rearrangement and 6 patients harbored JAK-STAT activated alterations in the Ph-like group. Median ageof patients in the Ph-like group, Ph+ group and B-other group were 21, 39 and 23 years old, respectively (P<0.001). There is no difference in gender distribution among the three groups. Patients in the Ph-like and Ph+ ALL group showed higher white blood cell counts at diagnosis (P<0.025). ALL patients accepted autologous anti-CD19 or anti-CD19/CD22 tandem CART cells infusion. The percentage of patients with active disease before accepting CAR T-cells infusion was 64.7% in the Ph-like group, 39.1% in the Ph+ group and 62.7% in patients with other B-ALL. 16/17 (94.1%) patients responded to CART therapy in the Ph-like group, including 11/17 (64.7%) MRD negative CR, 6/17 (29.4%) MRD positive CR. 22/23 (95.7%) patients responded to CART therapy in the Ph+ group, including 14/22 (60.9%) MRD negative CR, 8/22 (34.8%) MRD positive CR. 50/51 (98.0%) patients responded to CART therapy in the B-other group, including 28/50 (64.7%) MRD negative CR, 22/50 (29.4%) MRD positive CR (Table 1). Treatments and response evaluations were demonstrated in Figure 1. The estimated 2-year EFS in the JAK-STAT activated group and ABL1 class group was 70.1%±14.7% and 55.6%±24.8%, respectively (P=0.97) (Figure 2A). The estimated 2-year OS in the JAK-STAT activated group and ABL1 class group was 81.8%±11.6% and 83.3%±15.2%, respectively (P=0.67) (Figure 2B). The estimated 3-year EFS were 64.0%±13.7%, 55.5%±10.6% and 56.3%±7.1%, in the Ph-like group, Ph+ group and B-other group, respectively (P=0.799) (Figure 3A). The estimated 3-year OS were 65.9%±16.5%, 59.7%±10.5% and 61.6%±7.3%, in the Ph-like group, Ph+ group and B-other group, respectively (P=0.758) (Figure 3B). There were no difference in the severity of all grade of cytokine release syndrome (CRS) between 3 groups. Grade 3 CRS was detected in 11.8%, 13.0% and 23.5% of patients in the Ph-like, Ph+ and B-other ALL groups (Table 1).
ConclusionsIn this study, some Ph-like ALL patients showed resistance to traditional chemotherapy and targeted drugs. When anti-CD19 bispecific or anti-CD22 antibodies are not available, sequential anti-CD19 CART therapy followed by allo-HSCT will be an effective and important strategy for the treatment of Ph-like ALL.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal